Executive Summary
Fully realizing the social and economic benefits of halting COVID-19 requires investing in a fast and fair global rollout of COVID-19 vaccines. CARE estimates that for every $1 a country or donor government invests in vaccine doses, they need to invest $5.00 in delivering the vaccine.
Investments in frontline health workers are a critical component in this comprehensive vaccination cost. Of the $5.00 in delivery costs, $2.50 has to go to funding, training, equipping, and supporting health workers—especially women—who administer vaccines, run education campaigns, connect communities to health services, and build the trust required for patients to get vaccines. For these investments to work, they must pay, protect and respect women frontline health workers and their rights—a cost that is largely absent from recent WHO estimates on vaccine rollout costs. No current global conversations or guidance on vaccine costs includes the full cost of community health workers or long-term personnel costs.
Investing in a fast and fair global vaccine distribution will save twice as many lives as maximizing vaccine doses for the wealthiest countries in the world. Even better, investing in vaccine equality will speed up economic recoveries in every country in the world. For every $1 invested in vaccines in less wealthy countries, wealthy countries will see $4.80 of economic benefit because economies can fully re-open sooner. Failing to make this investment could cost wealthy economies $4.5 trillion in economic losses.
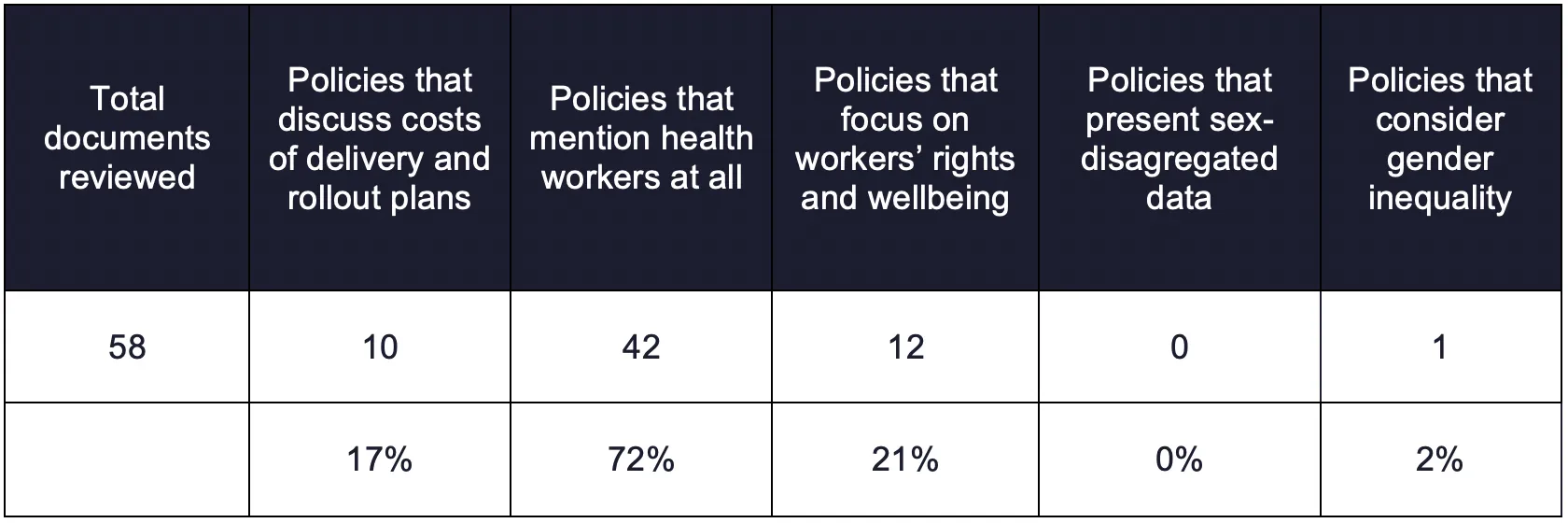
Current global debates are focused so narrowly on equitable access to for vaccine doses that they largely overlook the importance of delivering vaccines—and the key role women frontline health workers play in vaccine delivery. Of 58 global policy statements on vaccines, only 10 refer to the costs of delivery at all—and these are primarily technical advisories from the World Health Organization. No government donors are discussing the importance of vaccine delivery systems that are necessary to ending COVID-19. Only one statement—from Norway—refers to the importance of women health workers as part of the solution to ending COVID-19.
As new and dangerous strains of COVID-19 emerge in countries that are struggling to access the vaccine and control the pandemic, every day we wait for fair global vaccination allows for more contagious strains that spread around the world. The more chances the virus has to mutate in non-vaccinated populations, the higher the risk for everyone. Comprehensive global vaccine delivery plans that make sure the vaccine gets to people who need it—and that those people are ready to get the vaccine when it arrives—are the only way to end this threat. No one is safe until everyone is safe.
Since COVID-19 started, essential workers in hospitals have gotten much well-deserved attention as heroes who have helped control and manage the epidemic, care for the sick, and lose their lives serving others. Those heroes in health centers are only part of the story of how we’ll end COVID-19. Less recognized, but no less important, are the 3.5 million semi-formal and informal health workers around the world who serve the patients at the “last mile” of delivery. At least 70% of these health workers are women – who are risking their lives to get vaccines, services, and supplies to the most underserved and at risks populations in the world.
“The constant fear of my safety and survival has become a part of me, and I continue anyway. If not me and the many of like us reaching out, there are families who will not have one one to help them during this crisis. Nothing can stop me.”
– Karunya Devi, Social Worker and Project Manager in India
Appallingly, these women are getting little of the protection, recognition, equality, and pay that they deserve. Women health workers contribute $3 trillion dollars to the global economy every year, but HALF of this work is unpaid and unrecognized. Where they do get paid, they make 28% less than their male counterparts. They aren’t getting access to the vaccines, either. WHO estimates that currently 30 million high-risk people are not included in any government vaccination plans, and many of them are community health workers. In COVID-19, trauma and overwork are putting millions of healthcare workers at risk and compromising the care they can give. In the US alone, 76% of nurses are reporting burnout and exhaustion, and there are similar numbers in most countries in the world. Investing in these women is one of the best ways to ensure we experience the benefits of COVID-19 vaccines. Those investments will continue to payoff for years to come in pandemics avoided, faster crisis responses, and economic growth.
Respecting human rights, equality and leadership for women health workers is the key ingredient to keeping everyone safe from COVID-19. Women health workers have incredible insights about what is working, what patients are experiencing, and where there are gaps in the system that leaders need to quickly pivot to fill. Currently, they have few ways to share these insights in ways that improve the system. While evidence shows that having women frontline health workers involved in decision-making and shaping solutions improves life expectancy and patient outcomes, only 25% of leaders in the health care field are women. The lack of women in health care leadership significantly decreases the ability to effectively deliver vaccines and responses to COVID-19. It also holds back the potential of half the population and reinforces inequalities we should be dismantling.
Recommendations
We can solve these challenges if global leaders—especially high-income countries and multilateral donor agencies—focus on four key actions:
- Invest global funding in a fast and fair global vaccine rollout. High-income countries, donors, development banks, and national governments need to invest in comprehensive vaccine delivery. This investment has to include not just the money invested per dose of vaccine, but also an average of $5.00 in preparation and delivery for every $1 in vaccine. COVAX and WHO need to include the full costs of delivering vaccines, including all health workers—formal and informal—as part of their costing models and advocacy asks.
- Protect, pay, and value (women) frontline health workers. Out of the $5.00 in delivery costs, $2.50 has to go to equipping, paying, training, and supporting frontline health workers (at least 70% of whom are women). That includes ensuring they are first to receive the vaccine when available in their country and provided adequate personal protective equipment. It also includes ensuring equitable pay, and safe and supportive working conditions for women health workers on the frontline of COVID-19 response, including childcare, hazard pay, and funds for health-related expenses.
- Invest in women leaders. Ensure women, especially women frontline health workers, have meaningful roles and voice in leadership in shaping vaccine roll out, policies and programs at all levels.
- Start immediately to build national vaccine readiness and strengthen health systems so they are prepared to pivot quickly to fast and fair vaccine delivery, once doses are available.
FULL REPORT
No one is safe until everyone is safe
The COVID-19 pandemic has reinforced what the world already knew: diseases do not respect borders. With variants of the virus, such as those found in the UK, South Africa, and Brazil, continuing to emerge and spread in new countries, it is painfully clear that the safety of any person depends on the ability to protect everyone. While some countries begin to vaccinate their populations, we are not safe from COVID-19 until everyone is safe. Promoting justice and equality isn’t just the right thing to do, it’s also the only path through the pandemic.
We can save twice as many lives if we invest in a fair vaccine distribution than if we only focus on high-income countries. A study from Northwestern University estimated that 61 percent of global deaths could be averted if the vaccine is distributed to all countries proportional to population, while only 33 percent of deaths would be averted if high-income countries got the vaccines first. If we do not effectively reach lower income countries, especially vulnerable and marginalized populations within these countries, the long-term impact of COVID-19 will be catastrophic with global health, social and economic implications.
“It was terrifying to think about being a carrier of this deadly virus. I have four kids…It was scary to think that this could infect our kids.”
– Meagan Cundiff, Paramedic in the United States
Inequality risks all lives everywhere. COVID-19 may not respect borders, and it may put everyone at risk, but its impacts are hitting poor and underrepresented people hardest. In the United States and worldwide, the pandemic is having a disproportionate impact on people who are already face unfair obstacles due to race and ethnicity, gender, age, occupation, or other contributing factors. Global and national leaders can do better than this. We can act to support equality in ways that will protect everyone.
Stronger variants of the virus will continue to emerge in populations that are not immunized, and social and economic inequalities will only widen. Emerging mutations and variants of COVID-19 that emerge and spread in some countries will affect us all. They could reduce the efficacy of vaccines we do have and make it harder to reopen global economies in the ways that would jump-start a post-pandemic recovery.
No one recovers until everyone recovers
We have already seen COVID-19’s devastating economic effects on national economies, and the global economy. The global recession sparked by COVID-19 is also reversing the economic progress of several countries in various regions, with the threat of pushing 96 million people into extreme poverty, of which 47 million are women and girls. If we don’t quickly invest in a fair vaccination campaigns, we run the risk of prolonging a pandemic that has most detrimental consequences for the people who can least afford it. The pandemic sets our journey towards equal rights and equality back decades.
Investing in fair global vaccinations will have economic benefits for everyone. For every $1 they spend on vaccines in less wealthy countries, wealthier countries will get back about US$ 4.80 because their economies can reopen and grow faster. Even if wealthy countries had to spend $50 billion to support vaccinations in poor countries, it would still be a good investment in economic growth. If we fail to invest in a fair vaccine strategy, it could cost wealthy countries $4.5 trillion dollars, and economies like the US could lose 3.9% of their GDP. That risk impairs our ability to build a just and sustainable future.
Vaccines are useless without delivery systems
The current global debate about vaccine equality is largely ignoring a key ingredient in the solution to COVID- 19. No matter how many vaccines are globally available, investments in delivery of the vaccine are the only way to ensure everyone gets vaccinated and to control the pandemic. We must investing in comprehensive vaccination plans in all countries even before vaccine doses are available. Evidence from Africa shows that early investments in public health systems make the impacts of pandemics shorter and less severe. Despite this clear evidence from past pandemics, of 58 publicly available vaccination strategies and policy statements from global actors like the WHO that CARE reviewed, only 18% discuss the costs of vaccine delivery, and only one discusses the barriers that women health workers face in delivering vaccines.
“During Ebola, many of us health workers died… My advicce [to health workers] is to make sure you take care of yourself, think about your life first, about your family, and protect yourself.”
– Rosaline, Nurse in Sierra Leone
CARE estimates that to conduct a comprehensive strategy in this level of global pandemic, policy makers need to invest $5.00 dollars in rollout for every $1 they spend on vaccines themselves. Vaccines only work when patients receive them. That requires functional and equitable health systems that can reach people everywhere. What does that $5.00 include? To deliver vaccines effectively, for every $1 of vaccine, governments, donor nations, and multilateral funders need to invest:
- $2.50 to supporting health workers, including training, equipment, and salaries. This estimate includes fair pay and safe working conditions for both full-time health staff and part time workers, as well as surge capacity for vaccinators. Because of the particular crisis that COVID-19 has caused for women in terms of increased unpaid care responsibilities, this number includes $0.15 for childcare costs to make it possible for frontline health workers to function effectively. In addition to providing dignified and just work for health workers, this investment has long term payoffs for human health. Better trained, better paid workers deliver higher quality services and save more lives.
- $1.70 to strengthening and maintaining health infrastructure such as cold chains, vaccine tracking systems, power supplies, and administrative costs.
- $0.65 to social mobilization and education campaigns to increase vaccine acceptance.
- $0.15 to keeping health workers safe from COVID, including the increased time it takes to administer vaccine campaigns while enforcing social distancing and higher needs for personal protective equipment.
Methodology
We reviewed more than 100 published studies about vaccine costs. These studies are highly variable, and different studies include different costs of vaccination. There is no universally agreed standard on what costs to include in vaccination models. In particular, there are no guidelines about what costs to include for health workers of any kind or at any level. In this context, providing more information about the comprehensive cost of a fast and fair vaccine rollout is critical to advancing the global conversation. To arrive at the current cost estimate, CARE used WHO’s costing figures for a proposed Ebola vaccine strategy in 2016 as the basis for our model, adding other variables to that core model to ensure a more comprehensive picture. The proposed Ebola vaccination campaign most closely mimics the current context, having to quickly reach large segments of the population that are not included in traditional childhood vaccine systems with a new vaccine people may not be comfortable using. We complemented this model with cost estimates of how much implementing COVID-19 safety measures would increase the cost of a vaccination campaign. We also included standard systems costs for running long-term vaccination campaigns and supporting health workers from peer- reviewed published sources.
These figures are illustrative and based on global averages and large datasets rather than exact costs. They are intended to provide high-level guidance for planning vaccine campaigns and to inform current debates around vaccine equality, rather than to be inserted directly into budgeting plans. To plan costs for an actual vaccine campaign, policy makers will need to work closely with health financing experts and frontline health care workers in their own contexts. Specific costs will vary given the country context, the population demographics, and the existing health capacities and systems. The specific numbers may range from $3-$6 or even higher invested in rollout for every $1 invested in vaccines.
These numbers differ from the WHO estimate of $3.70 per person vaccinatedxxvi in several significant ways. First, CARE’s numbers aim to provide fair pay and safe working conditions for every health worker contributing to the vaccination effort—a cost that WHO has excluded from their estmates on the grounds that these costs already covered in existing health systems. We know that at least half of women health workers’ contributions to global healthcare are not currently paid, and we must include salaries and protection for these workers in global cost guidelines. WHO also estimates based on only formal health workers; CARE is advocating to include fair pay to ALL community health workers of all kinds—formal and informal—for their contributions to ending COVID-19. Finally, CARE includes contributions to support women health workers roles as unpaid caregivers to ensure women can both take care of their families and provide the essential services they support as health workers of all kinds. This explicit focus on overcoming women’s additional burdens is necessary to successfully ending COVID-19.
Only (women) frontline health workers make vaccinations possible
It is no surprise that the costs of paying, training, equipping, and supporting health workers are the biggest percentage of this cost estimate. We need to invest $2.50 in health workers for every $1 we invest in vaccines themselves. Health workers are the lynchpin in delivering fast and fair vaccinations all over the world. Despite this fact, frontline health workers (70% of whom are women) are chronically underpaid, undervalued, and often work in unsafe conditions without resources and support. Improving investments in these women will reinforce the ways that women frontline healthworkers make vaccines possible.
Build trust. A global study shows that at least 28.5% of people are heistant to take vaccines, and in some countries this numbers is as high as 60%. Without vaccine acceptance, we’ll never get enough people vaccinated to protect everyone. Investing in women health workers is the best way to overcome vaccine hesitancy. People’s trust in health care workers is one of the most important factors in improving vaccine uptake, more than the opinions family, friends or other non-medical sources.
Educate patients. Growing public mistrust could undermine the global effort on the development and coordination of distribution of COVID-19 vaccines. Fixing that requires investing in education campaigns to convince people that they should get the vaccine and help them figure out how to get one. It also includes promoting equality in vaccinations—and making sure that women and girls can access shots and other health services. At least 12% of total costs are educating people about the vaccine. Women frontline health workers are the ones who deliver most of that education.
Protect rights. Community health workers help communities hold service providers accountable and raise concerns that improve the quality, effectiveness, and uptake of health services. They protect patient’s rights, and help administrators find better ways to serve those patients.
Help everyone access vaccines and services. Women frontline health workers create solutions to the
many barriers women face accessing health care—like needing permission from their husbands or not being able to visit male doctors. These challenges have only gotten worse in COVID-19, where women are twice as likely to have lost access to health services as men are. Because women are primarily responsible for caregiving and their children’s immunization—and likely vaccinations for elderly family members in the COVID-19 context—these restrictions will dramatically reduce vaccine uptake. Women health workers have a unique ability to reach women in communities, understand the barriers they are facing, and plan solutions to overcome them.
Deliver vaccines and services. Women frontline health workers in Bihar, India got involved in planning vaccine campaigns and working with communities to improve uptake. Within 10 years, they’d improved vaccination rates from 12% to 84%.In Benin, women health workers have been able to combine vaccination and family planning services to build trust, dispel myths and misconceptions, and improve uptake.
Vaccinating just the 20% of the population that’s most at risk by the end of 2021 is the only way we know of to contain the COVID-19 pandemic. This is an urgent priority that will require 1.1 million full-time health workers, 770,000 of whom will likely be women. Achieving herd immunity- which will require vaccinating the 80-95% of people globally, that would require 4.4 -5.2 million full time health workers JUST focusing on vaccines and not delivering any other health services. That’s in a world that already had 18 million fewer health care workers than we needed to serve the people who need care.