The COVID-19 pandemic has delivered a devastating human and economic toll on the U.S.
Since the declaration of a global pandemic in March 2020 by the World Health Organization (WHO), more than 550,000 Americans and 2.8 million lives worldwide have been lost to the COVID-19 virus. This human toll has been compounded by significant economic disruptions and dislocations caused by the virus which, in turn, has amplified human suffering. Examples include:
- Historic contraction in economic activity due to both mandatory restrictions and voluntary changes in behavior by households and businessesiv
- Contraction in United States GDP by $800 billion to $1 trillion
- Job losses for 23 million Americans (at the height of the pandemic) with an additional 10 millionworking involuntarily on a part time basisv
- A 32.6% decrease in small businesses compared to January 2020
- Catastrophic losses to several sectors including airlines, cruise and hospitality, and retail
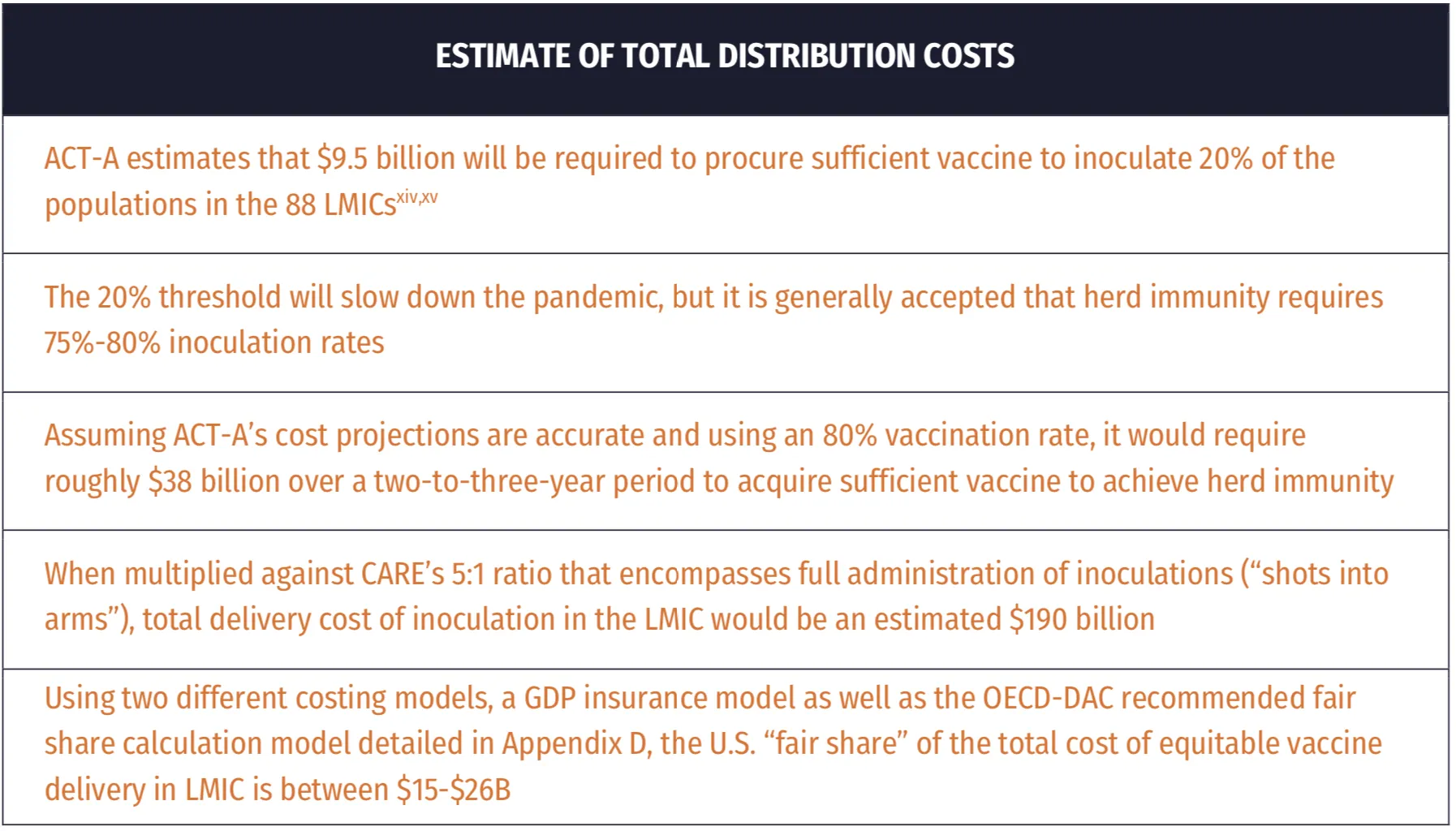
The economic harm to the U.S. will grow as the pandemic persists globally, potentially costing the U.S. economy an estimated $207B – $671B over the next five years.
In a highly integrated and tightly connected global economy, a prolonged pandemic will continue to negatively impact the United States economy. The ability to obtain or distribute intermediate inputs and final goods via global supply chains are all driven by interlocking trade relationships. Specifically, low- and middle-income countries’ (LMIC) infection rates can reduce foreign demand for products whereas economic lockdowns can interrupt supply chain flow.
Multiple studies have concluded that global equitable access to COVID-19 vaccines, or lack thereof, will have considerable impact on global economic stability and growth, significantly threatening the economic recovery of high-income countries like the United States. The results from one of these studies is described below and others are summarized in appendices.
A study commissioned by the International Chamber of Commerce (ICC) Research Foundation assessing the immediate economic costs of uncoordinated COVID-19 global vaccination that are solely due to international linkages concluded that a globally coordinated drive for the production and the distribution of the COVID-19 vaccine is necessary. It also emphasized that advanced economies have strong economic incentives to quickly support their trading partners in eliminating the pandemic locally. While this study has a higher estimated economic impact than others, it is more comprehensive. It highlights that if advanced economies are fully vaccinated but the current uncoordinated approach to global vaccine distribution continues, the world risks a global GDP loss of as much as $9.2 trillion in 2021 alone.
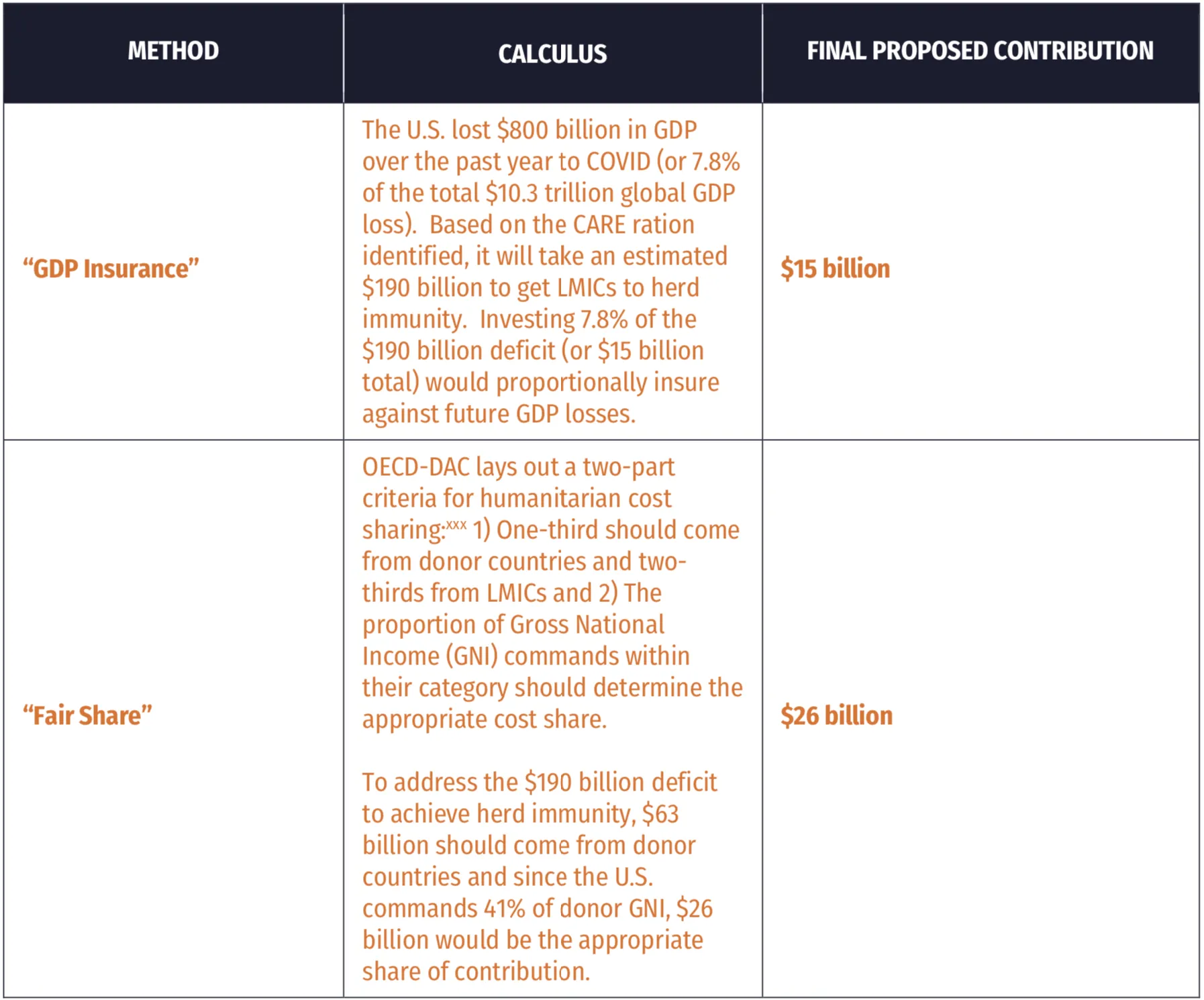
Furthermore, their estimates suggest that up to 49% of these costs will be borne by advanced economies, regardless of their own vaccination rates. In a scenario where developing countries vaccinate half of their population by the end of 2021, total global economic losses could be $3.8 trillion, $671 billion in the United States (3.14% of 2019 levels of GDP). In such a scenario, if the United States unilaterally bridged the World Health Organization’s Access to COVID-19 Tools Accelerator (ACT-A) funding gap, it would net a domestic return on investment of over 30.
Other analysis using more conservative models still project the potential damage done to the U.S. economy if we fail to achieve vaccine justice in LMIC to be in the billions of dollars. A study was conducted by the Eurasia Group to assess economic impacts of global equitable access to COVID-19 vaccines to 10 major economies. The results concluded that these economies would benefit by at least $153 billion in 2020–21 and $466 billion by 2025 (more than 12 times the $38 billion estimated total cost of the ACT Accelerator). According to their analysis, the US would risk $78.8 billion in economic benefits in 2020-21 and $207.1 billion at risk from 2020-25.
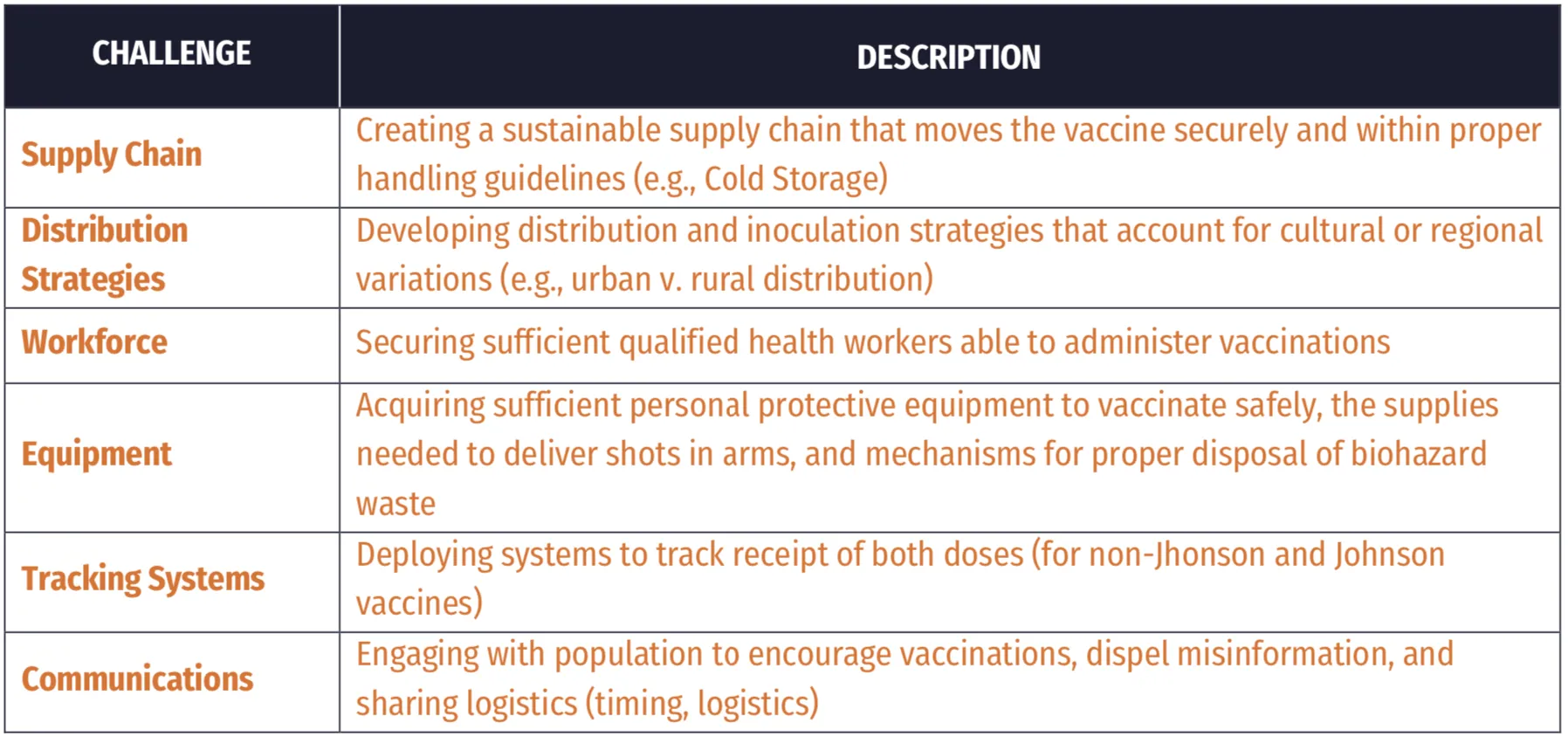
An effective response must be comprehensive, covering the acquisition of vaccines and getting those vaccines to the most vulnerable. And it must be expedited.
Effective mitigation strategies to end the pandemic globally will require a comprehensive approach to ensure that the most economically vulnerable nations receive sufficient assistance to fully vaccinate their populations and stem the potential emergence of variants. The greater the opportunity for the virus to transmit and multiply, the greater the likelihood that mutations and variants are produced. This natural process creates a race against time. The risk to public health is greatest when variants and mutations render vaccines ineffective. The best strategy to escape this cycle is to vaccinate as many people as possible in the shortest amount of time to reduce the number of potential hosts and reduce community spread. In addition, ongoing efforts in the United States are focused on researching the efficacy of existing vaccines against COVID-19 variants of concern; optimizing schedule, doses, and boosters; exploring safety and adverse efforts after immunization; and focusing on global surveillance for mutations. The intent of all these actions is to turn what is largely an unmanageable global pandemic into a more predictable, manageable endemic with less opportunity for viral mutation. But even as these efforts increase, strengthening health care services in LMIC settings will be a critical success factor in combatting COVID — the risks of viral mutation can occur anywhere in the world and result in immediate health and economic impacts for the United States.
Another important consideration is the speed of vaccination in LMICs, which will be uneven. In some countries, such as Rwanda, 95% of its COVAX doses were used because of the country’s robust investments in its health systems. On the other hand, Cote d’Ivoire has only used 10% of their vaccines in the same time frame. In addition, it will be critical to use existing, trusted vaccination institutions and processes developed over the past few decades in response to malaria and other diseases. This will allow countries to maximize the HIC financial contributions through efficient, effective, and equitable distribution of vaccines while also preventing against potential dangers associated with fraud and graft.